With the peak of the COVID-19 pandemic in Saskatchewan still on the horizon, health officials have rolled out a series of contingency plans which would be enacted to meet the projected healthcare needs of residents until heightened levels subside.
During a press conference on Wednesday, Saskatchewan Health Authority officials presented a trio of potential COVID-19 peak outbreak scenarios, and the accompanying facility and personnel changes which would be enacted to meet that need.
“This data is not for prediction of future, it’s data that acts as a planning tool to ensure that we’re preparing for the worst but aiming for the best,” explained Scott Livingstone, CEO of the Saskatchewan Health Authority.
A trio of “what if” scenarios were shared, with the predictive modelling scenarios approximating a high range, mid range and low range of COVID-19 infected persons. The high range scenarios calls for a peak total of 408,000 cases (34.7 per cent of Saskatchewan residents) along with the potential of 8,370 COVID-19 deaths. The mid range scenario calls for the possibility of a peak of 262,000 cases (22.3 per cent of Saskatchewan’s population) along with 5,260 deaths. The low range scenario is calling for a peak of 153,000 COVID-19 cases (13.0 per cent of Saskatchewan’s citizens) and the potential of 3,075 deaths.
“It is not a predictive model..but it does provide information to support both the response and the preparedness, and that was our key priority in using the dynamic modelling,” explained Dr. Jenny Basran, Senior Medical Information Officer with the Saskatchewan Health Authority.
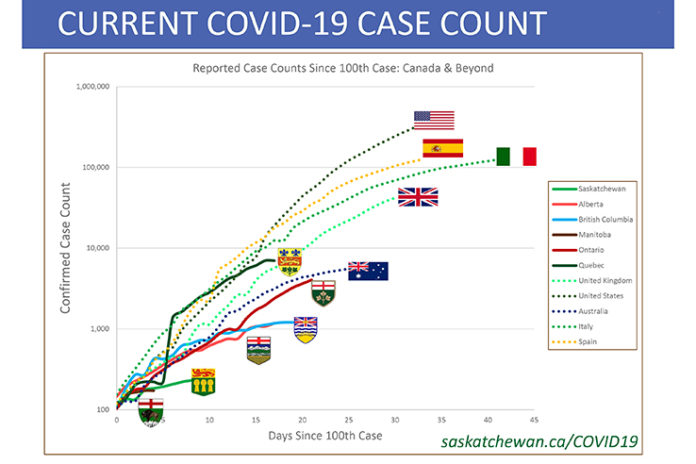
As a novel coronavirus, there is no past experience to learn from and apply to dynamic modelling. However, the dynamic modelling allows them to look at learnings from other jurisdictions and evidence they are sharing.
The high range analytic uses a basic reproductive constant of 4.0, and this high range peak would produce the hospitalization of 4,265 COVID-19 patients in acute care simultaneously, with 1,280 of these patients in the ICU at one time, with 90 to 95 per cent of those ICU patients requiring ventilation.
“They were looking at some of the Canadian data and there is a signal to suggest that the R0 (reproductive constant) potentially could be at 4.0. We’ve heard similar comments from our colleagues across the country,” Dr. Basran noted.
The middle range scenario was based on the low Italy range of a 2.76 reproductive constant, where they more prepared and the impact wasn’t as severe as the hardest impacted areas of Italy.
“We thought that it potentially could represent the situation here in Saskatchewan.”

Modelling estimates show the mid range scenario would at its peak result in 1,265 COVID-19 patients in an acute care hospital simultaneously. Of those hospitalized, 480 COVID-19 patients will be in the ICU with 90 to 95 per cent of those patients requiring ventilation.
The final scenario utilizes the reproductive constant of 2.4 experienced in Wuhan, the location where the virus had its first outbreak and where significant steps were put in place to lessen the impact of the virus.
At the peak of this low range scenario, 390 COVID-19 patients will require to be in an acute care hospital simultaneously. Of those hospitalized, 120 COVID-19 patients will be in the ICU with 90 to 95 per cent requiring ventilation.
“Again this is not predicting what will happen in Saskatchewan, it is applying those numbers in that situation to Saskatchewan. It is too early for us to know the exact scenario we’re in in Saskatchewan, and will really depend on how well we are comply with the Medical Health Officer and interventions,” Dr. Basran commented.
“Our anticipation and our hope is that we are doing even better than this,” she highlighted.
“The key message here is that dynamic modelling isn’t a prediction. We are not predicting that these are the numbers, but it does provide us with a range of ’what if’ scenarios. If this were to happen in Saskatchewan, what would the numbers look like and how would we plan both our public health response as well as our acute care planning. We do see from the charts that current interventions have made a difference and that’s really a key thing to identify. But the most important variable for us to save lives and healthcare workers is really the public’s compliance with isolation measures, physical distancing and washing your hands.”
There is a double strategy to deal with these modelled scenarios – preparing the healthcare system to accommodate additional patients, plus continuing initiatives designed to flatten the curve of the spread and allow the healthcare system to handle patients without spiking numbers of patients.
“My take away is that the models underscore the importance of aggressive and sustained public health measures and population health approaches that can help us flatten the curve,” explained Dr. Julie Kryzanowski, Senior Medical Health Officer with the Saskatchewan Health Authority.
As they know that individuals and communities will be effected in different ways by COVID-19, they are initiating a public health response that includes increasing testing, providing them with data identifying cases early so they can respond appropriately. There are currently 38 SHA testing sites across the province. Five assessment sites are in operation, with an additional 21 planned to open in the coming weeks.
They are also enforcing adherence to the Chief Medical Health Officer orders that are in place. Additionally they are investing in data tools that will help them to manage COVID-19 case clusters.
In the community they are making more primary care services available for everyday healthcare needs. They have expanded the HealthLine 811, with over 250 staff trained to provide telephone medical advice. They are shifting to a delivery of more services through virtual care models, which includes video conferencing and Telehealth options, with more than 750 clinicians set up to provide services in this way.
“As we move into the next weeks and months to come, we need to remember that all of these measures need to be sustained to be effective. Saskatchewan is early on it its path and response to COVID-19. We need to be staying strong and healthy by caring for physical, mental, social and spiritual health to be resilient as individuals and as communities. And we need to keep learning and understanding and removing barriers that are preventing people from taking the necessary actions,” Kryzanowski said.
“We do know that the pandemic will continue for weeks and months to come. We may not see the whole picture, or understand its full impact, until it’s over. But we need to be tracking these direct and indirect impacts as we go forward and building that into our planning and response,” she added.
The containment and delay strategy will help prevent community transmission and population health promotion will strengthen community and individual resiliency.
Derek Miller, Commander of Emergency Operations Committee, presented the details on how hospitals are gearing up to handle the projected surges of COVID-19 patients.
“Our response will be staged according to increases in demand. We intend to cohort, which means bring together in consolidated locations, COVID-19 patients as much as possible. This may be at the unit level or ward level within facilities. It may also be by designating facilities as COVID-19 hospitals,” Miller said.
“This is a provincial response. It’s not by facilities or silos within areas or geography. We are going to manage this though centralized bed flow coordination, air traffic control like coordination of patients to ensure that they are seeking and getting care in the right and best location.”
He noted that bed space has already been made available following the implementation of a province wide slow down of non-essential and non urgent services. This initiative has freed up more than 1,000 beds across Saskatchewan’s acute hospitals.
However, they are also planning up for a staged expansion of acute care capacity which will allow for an up to 57 per cent increase in acute beds as required. Intensive care beds will increase from the current 98 ICU beds up to 963 beds as needed during the response.
Additionally there are plans in place to preserve the supply chain, plus and a labour pool management strategy has been enacted to ensure the right healthcare workers will be in the locations they are needed to support the provincial response strategy.
The province has designated spaces in 20 Saskatchewan hospitals where COVID-19 patients will be treated, and they have created designated COVID-19, non COVID-19 along with mixed hospitals as demand dictates.
Creating additional community treatment capacity to manage any surges in demand.

In Southern rural Saskatchewan, this plan includes ICU capable COVID designed hospitals in Swift Current and Yorkton, along with 18 additional communities where COVID patients would be hospitalized. In this region those designated hospitals are in Maple Creek, Shauanvon, Gravelbourg, Assiniboia, Rosetown and Outlook.
The province is currently not activating contingency capacity at this point in time, and would only ramp up capacity if health officials see an indication they would need to scale up beyond their planned capacity.
Among Integrated Rural Health facilities, there is a currently a daily demand for nine of 14 available ICU beds, and only 349 of the available 698 Acute Care Beds are being utilized. If Saskatchewan approaches the higher range estimates, in Integrated Rural Health facilities they are planning to increase the number of ICU beds to 80, but if they reach a potential 236 ICU patients at the peak of the pandemic, their surge capacity in the rural area would fall 156 patients short.
For this reason they would direct critical care patients from rural centres to urban sites where additional capacity exists. Province wide they are gearing up for the potential of a need for 833 total ICU spots to handle the peak flow of COVID positive patients, so they could initiate plans to activate up to 963 beds to meet the surge capacity of 963 beds. Regina would have 410 of those beds, with 342 in Saskatoon. The north would have 131 spots, and 80 would be in rural Saskatchewan.
Similarly, Acute Care planned capacity would also need to increase, with a potential demand of almost 2,000 acute patients from COVID-19.
“The planning figures that we are pursuing for Saskatchewan is about 3,300 acute patients at the peak. We’ve established a plan within our existing facilities by expanding into different spaces where we could accommodate almost 3200 patients, which as you note is short of what we could anticipate at a peak. And therefore we’ve identified the need to establish two field hospitals to address this additional capacity. So we will be activating a field hospital in Regina and one in Saskatoon in order to give us the additional space in order to allow for the patient demand at the potential peak.”
Miller pointed out that Saskatchewan currently has 450 ventilators to meet the modelled demand which would exist in both the low and mid range scenarios which were presented. However a shortage would exist in the high range ‘what if’ scenario.
“We have identified a planned ventilator requirement of 860 ventilators to meet what we might anticipate at the planned capacity level. So this creates a gap of 410 ventilators.”
The SHA has confirmed they will receive an additional 200 ventilators in the short term, and 100 of those are expected to be delivered in the next two to three weeks. They continue to work to close that gap in order to be sure they are prepared with the right amount of ventilators.
Health officials are hopeful that existing community health measures are having enough of an impact that Saskatchewan can avoid a high range scenario.
“At this point in time we just don’t have enough data that’s going to tell us exactly when we’re going to see that peak or how long,” Livingstone said. “It’s important for everybody to understand the more you flatten the curve the longer we stretch this out. And that’s intentional. It’s so we avoid those peaks that we’ve seen across the world where healthcare systems are completely overwhelmed by COVID. And not just the COVID patients, but the not COVID patients are not receiving healthcare in the same way that they should be.”
“It is early. We have some optimistic signs, and our hope is certainly that we are on a better trajectory than our ’what if’ scenarios,” Dr. Basran said. “But at the current time we do not have enough information to be able to know for certain. And it’s important that our health system is ready. We’ve seen in other jurisdictions where it rapidly came upon them. And with not only the mortality and morbidity associated with COVID, but additional deaths due to a system that wasn’t able to anticipate and be prepared. So it was very critical for us to ensure that we are ready and that we have a sense of the scope of the potential issues.”
Dr. Shaw concluded the media availability with a poignant message for all Saskatchewan residents.
“The most important variable in saving lives and protecting our healthcare workers is your ongoing commitment to the public health measures – including self isolation when directed, practicing physical distancing, effective hand hygiene, and staying home whenever and wherever possible. We cannot change the virus, but we can control how the virus spreads. Following these practices will save lives, and it will protect our healthcare providers to ensure that we are there when you need us.”
“Normally we are here to help you. And now we need you to help us. I am asking you to continue to do what you’ve always done as Saskatchewan people – come together in a time of need.”
“This message is for every resident of Saskatchewan. You have the opportunity to save lives. Please take it.”