The Saskatchewan Health Authority (SHA) released a new pandemic model which shows the province is in a “significantly better” position to manage COVID-19.
The SHA revealed their second modelling scenario on April 28, with the impacts of Saskatchewan residents flattening the curve resulting in significantly different numbers than the pandemic modelling released on April 8.
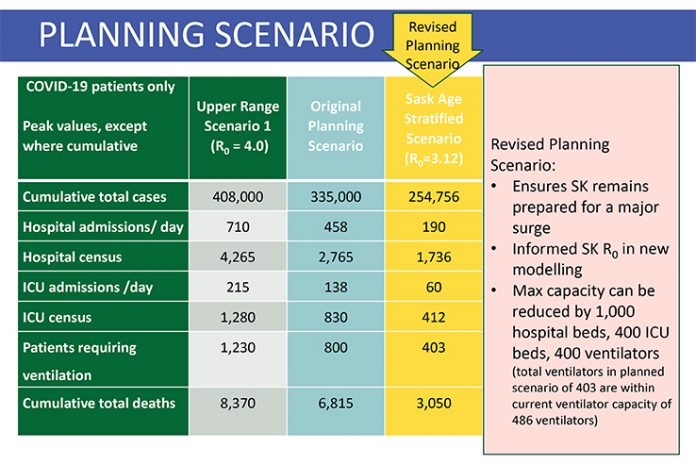
The new scenario calls for an estimated 1,000 fewer hospital beds, a reduction of 400 ICU beds, plus 400 fewer ventilators than the original planning scenario from earlier in the month. Their initial projections were based on a Basic Reproductive Number of 3.12 (the average number of people a single COVID-19 patient could infect), while the significant public health measures taken in Saskatchewan have resulted in an Effective Reproductive Number of 0.7 in the province as of April 25.
“We are adjusting our planning to align with these new figures. It will ensure that we remain prepared for a major surge. It is based on Saskatchewan data and information, and we believe it is more reflective of a potential scenario,” explained Derek Miller, Emergency Operations Centre (EOC) Lead for the Saskatchewan Health Authority.
The most recent planning scenario is based on the province experiencing 254,756 total COVID-19 cases, down from their previously modelled number of 335,000. It also drops the daily hospital admission numbers to 190, a reduction from the previous scenario of 458 daily admissions. Similarly, the number of daily ICU admissions is now set at 60, a decrease from 138. The current scenario is planning for a total of 3,050 total deaths, over half the previous scenario suggestion of 6,815. The revised scenario also anticipates the need for 403 ventilators across the province, which falls within the current provincial capacity of 486 ventilators.
“It’s important to look at this as a worst place planning scenario not as a projection or a prediction of what will come. We all really hope that we don’t see anything like this, but we need the system to be able to be prepared to actually respond should this happen,” Miller added.
Saskatchewan Health Authority CEO Scott Livingstone also noted this modelling used for a planning scenario isn’t a crystal ball, and their first scenario took statistics from other countries. However, Canada has experienced its own challenges with COVID-19.
“Since those days we’ve seen things happen across this country in Ontario, Quebec, and right next door to Alberta, that is sobering to say the least with respect to how the system is preparing itself.”
He noted that despite re-opening plans, Saskatchewan’s medical system will continue to plan for a surge in cases.
“As we move forward with COVID, it’s not going away any time soon. So we’ve flattened the curve. That doesn’t mean COVID goes away. We’re going to be flat for a while if we can keep up this good work, and we’ll know that by the modelling that we’re doing. But we do know from the modelling if you withdraw for example a major component of public health orders of public distancing, the case numbers projected go right up to one of the worst case scenarios.”
Saskatchewan’s encouraging numbers are also prompting the SHA to begin exploring the logistics of resuming the non-essential medical procedures which were put on pause back on March 23. That original discontinuation of non-urgent/elective surgeries, procedures and diagnostics was implemented by the SHA in order to redeploy nurses and other staff, while also ensuring medical supplies and personal protective equipment was available when needed and to reduce the risk of further exposure to patients and healthcare workers.
Livingstone noted that the SHA is a complex healthcare system so it is not easy to quickly gear up these non-essential procedures, while similarly maintaining the ability to shift directions if something unpredictable happens.
“We have to prepare knowing that COVID is going to be with us for months. And we have to prepare knowing the system needs to restart, but at the same time we need to build that capacity. And even if we’re not using that capacity for COVID, we may need that capacity for other types of care that we will be providing residents to ensure the system smoothly goes back into full operation.”
While the Saskatchewan Health Authority along with the Ministry of Health are currently looking at the development of a health service resumption plan, there are no dates being discussed for these resumed services.
“This would be based on a phased approach. We are looking at community services, elective surgeries, and diagnostics that were impacted by the service slowdown that was introduced last month. It would be a cautious and methodical approach to reintroduction of services.”
The resumption plan development includes factors such as a prioritization of highest patient need, the risk of COVID-19 transition, looking at the impact that resumption of services would have on COVID-19 surge demand, plus PPE inventory.
Livingstone pointed out that approximately 3,800 surgeries delayed or postponed because of the gearing down of the system. Additionally, people were not going to the emergency room or to see their physicians during the pandemic distancing initiatives.
“We saw people shying away from hospital, shying away from healthcare providers cause we’ve created some fear across the province. And with that we know that there’s people that haven’t attended facilities when they probably should have. We’re starting that happen more.”
“Until we know and have assessed what’s gone on with those people that are out there – whether its a delayed elective surgery or a delayed procedure, or somebody just not being able to see their family physician on a regular basis to see how their chronic disease is doing – you won’t see us define an exact time frame.
“What we’re trying to do now is, just like we have with the data modelling, is use data to help inform where the best place to open up the system, carefully. But also to address the highest needs in our population. The last thing we want to do is start burning through elective surgeries only to have our facilities fill up with medical needs that we haven’t met, or diagnostic needs that went postponed.”
He said the phased in approach for elective surgeries will be similar to the re-open Saskatchewan plan, as it will be slow and methodical, while placing an emphasis on being able to provide broader healthcare and be ready for COVID patients.
“We see empty beds, and there’s lots of healthcare providers out there that are both concerned about what’s happening out there in the healthcare community. But also at the same time, COVID is not gone.”
“We can’t burn all our capacity to care for patients that we’ve postponed. We need to maintain that COVID capacity, and that’s what we’re going to continue to do just in case something happens,” Livingstone said of this front of mind decision.